ADHD Medication Rebound Recovery: 5+ Tips for Managing ADHD Kids’ After School Crash
Jul 02, 2025Billy stomps into the house and collapses onto the couch in a stupor. Or he bursts through the door climbing the walls. His stimulant medication has worn off and the adderall crash afternoon has arrived. Irritability spikes, difficulty focusing come back at full force, impulsivity reigns, and emotional overload follows. How are you supposed to get him to do homework, chores, or anything at all?
As a pediatric occupational therapist, mom and wife of those with ADHD, and certified ADHD rehab service professional, medication rebound is something I am intimately familiar with. I always prepare my families for this when they tell me their child has just started stimulant medication. Here are my best clinically informed, evidenced-based, and parent‑tested tools for after‑school stimulant rebound that combines an occupational‑therapy lens, sensory‑first strategies, and immediately actionable routines you can use today.
Author: Devina King, Occupational Therapist and Certified Autism and ADHD Specialist. Last updated: 1/1/2026
Table of contents
-
Nutrition and fuel to manage adderall comedown and ritalin crash
-
Routine and timing adjustments for ADHD morning routines and after school crash
-
Environmental and sensory supports for dysregulation and emotional overload
What is the ADHD medication rebound effect?
Medication rebound, sometimes called the ADHD medication crash or ADHD med rebound, happens when stimulant levels fall and symptoms return stronger than before. This ADHD medication rebound effect peaks just as afterschool restraint collapse begins. You can learn strategies for afterschool restraint collapse here.
Underneath that rebound lies a dopamine crash that worsens dysregulation. Adderall crash depression, Adderall comedown anxiety, and Adderall mood swings are common symptoms your child may have. Ritalin users experience similar Ritalin comedown and Ritalin crash patterns. No matter what stimulant your child is taking, these strategies to prevent and ease rebound will help.
Dopamine is the brain’s primary chemical for attention, motivation, focus and executive functions such as planning, impulse control, working memory and cognitive flexibility. It signals reward expectancy and drives engagement with tasks that might otherwise feel effortful. Adequate dopamine levels also supports emotional regulation by smoothing mood transitions and preventing overwhelm when stress peaks. When children with ADHD use stimulant medication to boost dopamine they experience clearer attention and stronger self control. As those levels fall the resulting dopamine crash can undermine all these processes at once. You can learn more from the National Institute of Health about the research behind how dopamine signaling in the brain’s reward circuits influences attention, executive functions and emotional control, and the neurochemical basis of behavioral regulation here. When you're child is in a state of reduced dopamine levels they probably require extra scaffolding for Impulse control difficulties, you can learn more strategies to help with impulse control here.
No matter what stimulant your child is taking, these strategies to prevent and ease rebound will help.
Nutrition and fuel to manage adderall comedown and ritalin crash: The ADHD brain needs more fuel
The brain is the hungriest organ in the body. It uses roughly 20 percent of our total glucose supply to power high-order tasks such as attention, working memory, and emotional regulation. In children with ADHD, fluctuating dopamine levels and less efficient neural signaling increase the demand for steady fuel. When blood sugar dips, fatigue, irritability, and difficulty focusing quickly follow. Stimulant medications suppress appetite while boosting cognitive energy needs. As the medication wears off, hunger returns with a surge. Without rapid access to quality fuel, children can spiral into low blood sugar and intense cravings. This cycle deepens the ADHD medication rebound effect by undermining executive functions exactly when after-school demands begin. Discuss any changes listed below with your child's pediatrician.
In his 2012 Burnett Lecture on how to treat ADHD based on science, Dr. Russell Barkley a renowned expert in ADHD, recommends that if you child is doing a task that requires a lot of executive functions (such as a test, homework, etc.) they should be sipping on sugar water (natural sugars are preferred such as juice compared to refined sugar). This is because this is the quickest way to get glucose available for the brain. You can watch the 2012 Burnett Lecture video where Barkley explains this here.
Discuss if low doses of caffeine may be safe for you child with their pediatrician. You can find a guideline for cardiologist's recommendations on safe usage of caffeine in children here. It may seem counter intuitive to give your hyperactive child caffeine; however, for many people with ADHD caffeine can actually calm them down and help them focus. You can read one research article in Current Developments in Nutrition that shows it helps children with attention, cognition, and impulse control here.
I remember one time my nephew who was undiagnosed ADHD at the time was struggling, and I asked his mom if I could give him my caffeinated drink and explained why. It helped immensely and he sat down and did his homework in 10 minutes for the first time in his life. That was the first of many times I provided my nephew caffeine when I noted he was bouncy, impulsive, and close to a meltdown.
-
High-protein snacks: Offer protein-rich bites at rebound time: cheese cubes, peanut butter crackers, Greek yogurt. Protein stabilizes blood sugar and sustains focus. For kids who prefer specific textures, try crunchy roasted chickpeas or a smoothie with nut butter. A common side effect of stimulant medications is reduced appetite. Something like a protein drink, pediatric meal replacement drink, or smoothie can be a way to get quick, quality nutrition when appetite is a struggle. Ensure is my go to when I am too tired to eat and I'm tired because I need to eat! You can learn more strategies for dealing with poor appetite by ADDitude here.
-
Green tea with honey: Brew a mild green tea sweetened with honey. The gentle caffeine lift supports attention, while honey delivers quick glucose.
-
Balanced meals: Balanced meals with complex carbohydrates, healthy fats, and lean protein at breakfast and lunch delay the onset of ritalin comedown and adderall crash symptoms. Also, learn more about why you should avoid things high in vitamin C such as orange juice within an hour of taking stimulant medications here in this stimulant medication side effect Q&A by ADDitude here.
Routine and timing adjustments for ADHD morning routines and after-school crash
- Booster doses and timing: Work with your child’s provider on a small “booster” short-acting dose 30–60 minutes before the crash window. This smooths blood-level dips and extends coverage into homework time.
- Scheduled downtime: Carve a 10-15-minute transition slot after school. A brief walk, stretching sequence, or quiet reading buffer helps shift from school demands to home life.
- Homework during peak coverage: Whenever possible, tackle heavier tasks such as math or writing while medication is still fully active. Reserve creative or physical homework for later.
- Maintain consistent ADHD morning routines: Keep steady wake-up times and dosing schedules to prevent severe Adderall comedown and difficulty focusing. You can learn more about how to help children with ADHD with morning routines here.
Environmental and sensory supports for dysregulation and emotional overload
- Design a calm corner: Create a low-stimulus zone with soft lighting, noise-cancelling headphones, or a weighted lap pad. A designated chill space signals it’s time to unwind.
- Hydration station: Keep water and electrolyte drinks at hand. Stimulant medication can also lead to dehydration. Dehydration intensifies fatigue and irritability. Even small amounts of dehydration can have huge effects. You can learn more about a study by University of Connecticut’s Human Performance Laboratory that shows that here.
- Calming tools: Offer stress balls, chewy necklaces, or textured fabrics. These sensory tools can redirect rebound restlessness.
- Visual schedules and timers: Use clear charts or phone alarms to signal snack, booster dose, and homework windows. Predictability reduces anxiety.
Physical and relaxation techniques to ease dopamine crash
- Light exercise breaks: Encourage jumping jacks, tossing a ball, or a quick bike ride. Physical activity releases endorphins and dissipates stimulant-wear-off jitters. You can learn more about the research demonstrating the bidirectional nature between exercise and dopamine here. Make sure to meet the child's energy level where they are and slowly transition them to where you want them to be. You can learn more about arousal transitions here.
- Mindful breathing and stretching: Practice deep-breath sequences or simple yoga poses together. Regular rehearsal ensures kids can self-soothe when rebound hits.
- Progressive muscle relaxation: Guide your child through tensing and releasing muscle groups, helping them tune into bodily tension and ease it.
- Offer a dopamenu: A dopamenu is a list of activities a child can do to raise their dopamine levels.
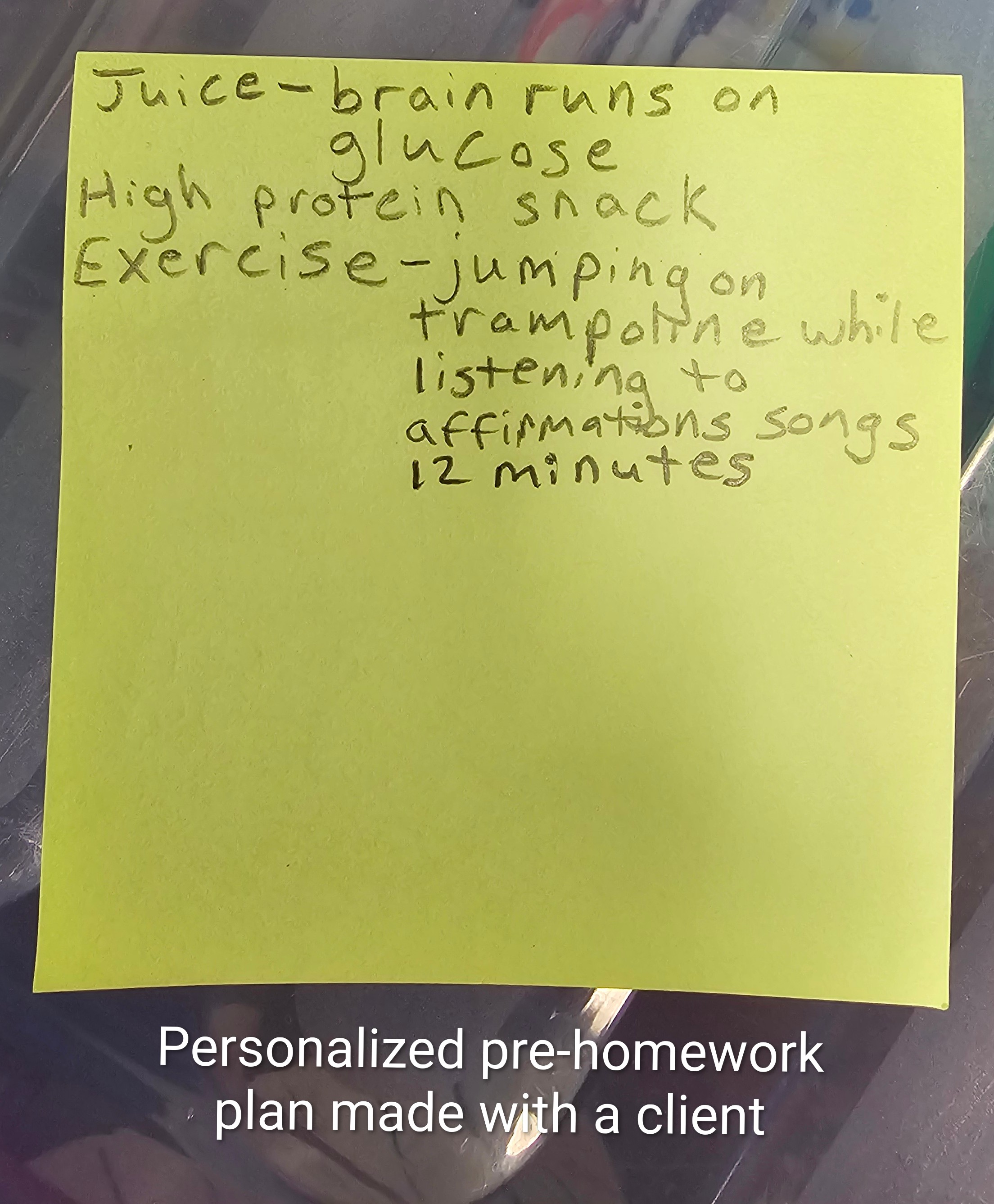
- Create a custom crash playlist: Across the board my ADHD or sensory seeking clients love this metal binaural beats song (no words) that you can find here and it really helps them focus to get homework done. One of my clients asked me to make her a playlist of affirmations songs because she gets stressed and starts saying mean things about herself when homework time comes and this has been very helpful.
Collaborative planning and communication
- Open check-ins: Ask one focused question, “How hungry are you right now on a scale of 1–5?”, instead of overwhelming them with a barrage of questions. Using collaborative problem solving to co-create plans and afternoon routines.
- Coordination with school and provider: Share crash timing patterns and ADHD medication rebound symptoms with teachers and prescribers. In our family my husband experienced such severe adderall crash symptoms that he was nearly impossible to hold a conversation with and forgot entire evenings. We worked with his prescriber and changed to an extended release dose; although we eventually had to stop all stimulant medications for other reasons. Tracking symptoms is really important in collaboration with providers. My husband uses the Human Health Tracker app which he finds really useful and intuitive for tracking patterns.
Every child’s rebound looks different. Tweak snack timing, experiment with green tea versus cocoa, and adjust booster doses under medical guidance. With a blend of nutrition, sensory supports, and strategic timing, you’ll transform afternoon crashes into calmer comebacks. You’ve got this.
FAQ
What is ADHD medication rebound?
Medication rebound, sometimes called the ADHD medication crash, happens when stimulant levels fall and symptoms return stronger than before. It often peaks in the late afternoon, just as after school restraint collapse begins.
How long does rebound usually last?
Rebound typically lasts about 30 to 90 minutes, though intensity varies by child, medication type, and dosage. Some children experience only mild irritability, while others have more severe emotional or behavioral crashes.
Is rebound a sign the medication isn’t working?
No. Rebound is a timing issue, not a failure of the medication. It occurs when stimulant levels drop quickly, leaving the brain temporarily under‑supported. Adjusting timing, dosage, or formulation often helps.
Why does dopamine play such a big role in rebound?
Dopamine supports attention, motivation, impulse control, and emotional regulation. When stimulant medication wears off, dopamine levels drop quickly, leading to irritability, impulsivity, and emotional overload.
How can nutrition help with rebound symptoms?
The ADHD brain needs steady fuel. Offering protein rich snacks, balanced meals, or quick glucose sources like fruit or juice can stabilize blood sugar and reduce irritability. Discuss any changes with your child’s pediatrician.
Can caffeine help children with ADHD during rebound?
For some children, small amounts of caffeine can calm hyperactivity and improve focus. Always consult with a pediatrician before trying caffeine, as safety depends on age, health, and dosage.
What routines reduce after school crashes?
Booster doses (under medical guidance), scheduled downtime, and tackling homework during peak medication coverage can smooth transitions. Consistent morning routines also prevent severe crashes later in the day.
What sensory supports are useful during rebound?
Calm corners, hydration stations, stress balls, weighted lap pads, and visual schedules help children regulate. Predictable sensory tools reduce overwhelm and provide safe outlets for restlessness.
How does exercise or relaxation help with dopamine crashes?
Light exercise releases endorphins and helps dissipate stimulant wear off jitters. Breathing exercises, yoga, and progressive muscle relaxation ease tension and support self regulation.
What is a dopamenu?
A dopamenu is a list of activities children can choose from to raise dopamine levels naturally. Options might include listening to music, drawing, or short bursts of movement.
How should families collaborate with schools and providers?
Share rebound timing patterns with teachers and prescribers. Track symptoms consistently and adjust routines or medication under medical guidance. Collaboration ensures supports are aligned across home and school.
Does every child experience rebound the same way?
No. Each child’s rebound looks different. Some may become irritable, others hyperactive, and some withdrawn. Tailoring nutrition, routines, and sensory supports to your child’s unique profile is key.
Can occupational therapists help with medication rebound?
Yes. Pediatric OTs provide sensory strategies, regulation tools, and environmental supports that ease transitions. They also coach families on routines and collaborate with providers to align interventions.
What caregiver strategies are most effective?
Simple check‑ins, collaborative problem solving, and predictable routines help. Asking one focused question such as “How hungry are you right now?” avoids overwhelming children and builds connection.
Should children take medication breaks to avoid rebound?
Some families consider “medication vacations.” This should only be done under medical guidance, as skipping doses can worsen symptoms or disrupt consistency.
Is rebound worse with certain medications?
Both Adderall and Ritalin can cause rebound, though timing and intensity differ depending on formulation. Extended release versions may reduce severity, but individual responses vary.
About Devina King, B.A. Psy, MSOTR/L, ASDCS, ADHD-RSP
Devina is an autistic occupational therapist, parenting coach, author, and credentialed autism and ADHD specialist with over 17 years of experience working with children, specializing in behavioral regulation and neurodivergence. As both a clinician and a parent, she combines professional expertise with personal experience parenting neurodivergent children who previously struggled with behavioral disorders. This unique perspective allows her to bridge the gap between science and real-world application, offering compassionate, evidence-based behavior treatment strategies that empower children to thrive.
You can learn more about Devina's credentials, lived experience, and approach here.
Publications
Devina has written many books. Her book From Surviving to Thriving: The Art and Science of Guiding Children to Develop Behavioral Regulation available on Amazon here, provides actionable insights for parents, educators, and professionals looking to support children in building essential self-regulation skills. Devina is an AOTA approved professional development provider. Reviewers praise her works for her comprehensive, refreshing and practical, compassionate approach that takes complex psychological concepts and evidence based approach and breaks it down into concepts anyone can understand and apply. Devina has been included in publications such as this article in Psychologist Brief available here and this article in Doctors Magazine available here. Stop by her store here to explore her latest resources, workshops, CEUs and parent coaching sessions designed to help children succeed in their behavioral development journey!